Insurance Based Care
We are embarking on a topic that often seems murky, convoluted, and controversial. But, as always, the effort and aim is only to inform and educate. Our overall goal, and hope is to improve the quality of care offered and see more Alaskans healthy and functioning optimally.
Over 70% of Americans are dissatisfied with our current system of care and believe the current system is failing to meet their needs (Harris, 2023).
High costs, limited insurance, and subpar preventive wellness measures rank among Americans' grievances.
But, when we take a deeper look at the traditional model of healthcare, it's easy to see why our current system of care is failing to meet Americans needs.
To put it simply, our system of care has become insurance based, rather than evidence based health care.
As most well intentioned models, health insurance originated for protection of patients and appeared at the beginning of the 20th century, toward the end of the industrial age and beginning of the Great Depression. During the industrial age the risk of employee injury grew, with very little support for employees and limited risk to employers. As a result, workman's compensation was instituted (Morrisey, 2013).
"Organized medicine supported the workers’ compensation legislation apparently under the view that injured workers would go to their family doctor for care, and the doctor would be paid by the workers’ compensation fund. Instead, however, employers began to directly retain and sometimes employ physicians to provide care. As a result, the majority of local physicians saw a reduction in the demand for their services. Those who had employer contracts did better, of course." (Morrisey, 2013)
This began to shift the model of care offered in the Western world.
Up to that point, family practitioners were deeply embedded in communities and would visit families directly in their homes for check ups. At the time, complementary medicine was practiced, as many family physicians would use known and accepted home remedies and holistic practices with emerging evidence based medicine. House calls were widely popular until the 1960's, but primary care began shrinking following World War II.
With the Great Depression hospitals saw an increase in acute situations in lower economic streams, but physicians wanted a proactive way to offer care (Morrisey, 2013). The Baylor Plan initiated in 1929, as the conception of Blue Cross, though it didn't transition to that title until 1934. The Baylor Plan was prepaid services offered for public employees (NIH, 1993).
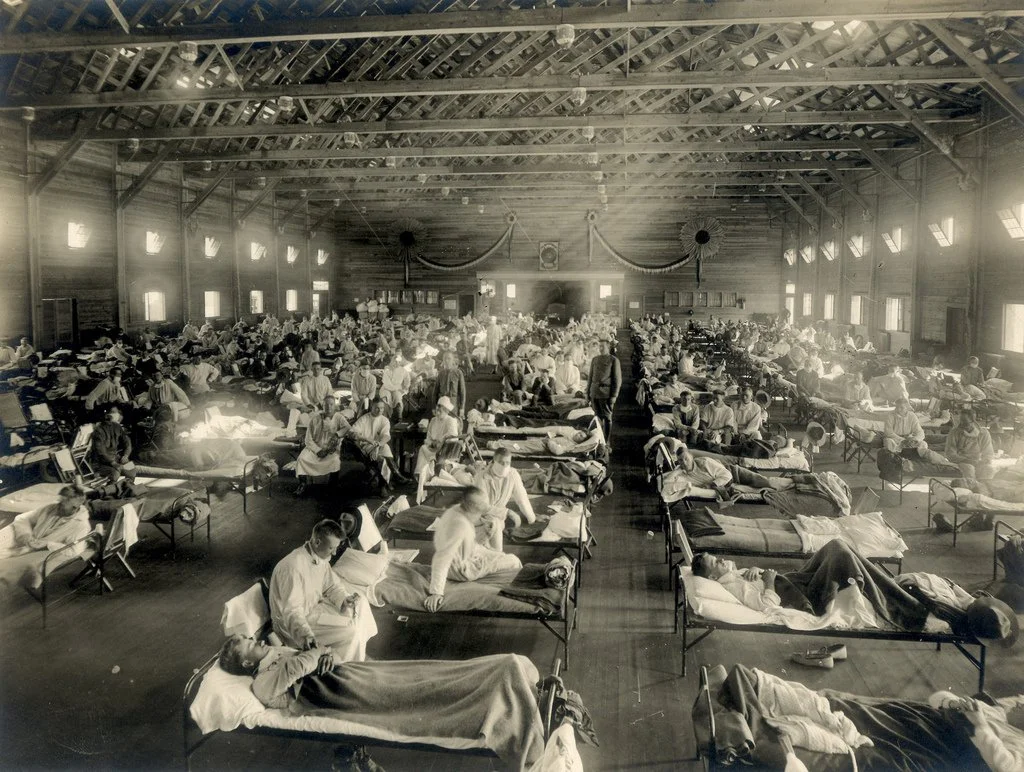
Emergency Hospital during influenza epidemic, Camp Funston, Kansas. (NCP1603)
While health insurance models and practices had existed since the Great Depression, states were not offering insurance models.
"Most states viewed the new hospital service plans as the prepayment of hospital services, rather than as insurance. In 1933, however, the New York state insurance commissioner determined that the plans should be viewed as insurance... The plans collected payments in advance and promised to provide care at some future date, not unlike life or casualty insurance. The upshot of this ruling was that the new health plans were required to comply with existing insurance laws; particularly, they had to have reserves to meet future claims." (Morrisey, 2013)
It wasn't until after World War II that the system began to grow. This is primarily because employers were "allowed to offer fringe benefits like health insurance for up to 5 percent of a worker's wages" (Moseley, 2008).
However, with the growing prepaid services becoming popular, physicians became concerned about the threat of insurance competition from Blue Cross. The primary concern being that a third party (Blue Cross) would lower their incomes by restricting their ability to set their own fees. Ironically, this led to the establishment of a network of their own insurance plans covering their services, Blue Shield to preempt the hospital based plans, Blue Cross, from taking over the primary care sector.
What is fascinating is that as insurance enrollment grew, primary care shifted and changed.
Even by the early 1980's, the majority of primary care practices were small and independent of hospitals. Providers were organized around relationships, patient loyalty, reputation, and a "pay what you can" fee-for-service (FFS) still existed. Primary care was family based care, personalized, comprehensive, with continuity and access to physicians.
"By the start of the 21st century, most primary care practices would be almost unrecognizable to past generations of primary care clinicians. Relative to decades ago, practices today are larger (Liebhaber and Grossman, 2007), often part of health care systems (Kane, 2019), and generally not organized around values, professionalism, and relationships."
The devolution of care follows the growth and expansion of insurance influence over medicine. Instead of personalized, comprehensive, evidence based care, 92% of Americans have now been enrolled into a system that is ineffective at disease prevention and cures.
With 1 in 2 Americans diagnosed with a chronic disease, and 1in 4 Americans with more than 2 chronic illnesses. (NCCPPHP, 2016) The US continues to spend the most money on health care, with the lowest results. In fact, the US leads the Western world in cost of care and chronic diseases. You would expect that with $4.5 trillion spent on health care (CMS, 2023), Americans would lead the world in health rather than disease states (NIH, 2019).
One of the primary reasons we see this is because the overwhelming number of Americans have been influenced to believe that insurance based care is the only option available.
But again, as health insurance continues to grow in influence, actual health care has continued to devolve.
Additionally, health insurance is the only form of insurance Americans have grown accustomed to expecting an insurance to pay for maintenance and prevention.
No other form of insurance, car, house, etc, do we expect to pay for the maintenance and upkeep of what is insured.
For example, if car insurance worked like health insurance, we would use car insurance to pay for our oil change, our gas, our filters, replacement of brake pads, etc. Car insurance companies would then create a network of mechanics that would offer the services the car insurance company would pay for. Customers would be limited to what mechanic and what forms of maintenance would be performed on their car. If you preferred synthetic oil, but your car insurance would only cover regular oil you would be bound to get regular oil. This could change the life expectancy and operation of your vehicle.
Health insurance was originally founded to proactively address health concerns and be available for traumatic events, similar to how we use every other form of insurance.
Unfortunately, we've adopted this model of care and as a result we've assumed reimbursement based care rather than evidence based, preventative, quality care and compromised the system. And sadly, much of our adoption of this form of care has been based primarily on fear.
Most of us know the importance and fundamental concept of insurance, care available for catastrophic events, but health insurance has grown beyond catastrophic care and now dictates, without many of us realizing it, our quality of care. Insurance based care is no longer serving providers or patients, but it is a fantastic business model for insurance companies.
Insurance has deviated from the original concept of offering safety for patients, to more costs, restrictions, and limitations. Sadly, most patients don't realize that the quality of their care is not influenced by the provider, but their insurance. While the 80's primary care was booming, a shift began to move away from longer visits to shorter cost effective visits. In 2007 the recorded average time primary care physicians spent with patients was 17.4 minutes (Tai-Seale, 2007). It is speculated that time has even begun to lessen.
Well intentioned people often ask us if we accept insurance, but we do not. There are several reasons, the primary being, we want you to receive quality care that you want. We want to turn over the ownership and influence of health to you working in tandem with providers. This is also why our concierge medicine visits are 45 minutes to and hour. We want you to have quality time with your provider to establish a relationship and come up with an effective plan.
Sadly, many people determine where to receive care based on their insurance, or if the business accepts insurance, without realizing the quality of care, thoroughness of diagnostics, and benefits of medications/supplements are heavily influenced by your insurance provider, with little research or evidence. As Chris Kresser said, "Insurance based care is reimbursement based care."
Insurance based care is not working for us, we need to make changes to receive the care that is best for our long term health.
It won't be easy, but we believe it's more than worth it to proactively care for your health. We need care that gets back to quality, evidence based practices that are patient driven and provider guided. We hope to get back to partnerships between providers and patients that end in actual health care.
We hope this only begins the conversation, and the effort many of us will need to make if we want to see the care we need and deserve. We are continuing to research efforts and ways for you to achieve the care you need in the future. Together, we believe we can begin to move the needle toward long term, preventative actual health care.
References
Harris Poll, 2023, The Patient Experience: Perspectives on Today's Healthcare
Ducharme, 2023, Exclusive: More Than 70% of Americans Feel Failed by the Health Care System
NIH, 2021, Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care
George B. Moseley III, 2008, The U.S. Health Care Non-System, 1908-2008
NIH, 2013, U.S. Health in International Perspective: Shorter Lives, Poorer Health
NIH, 1993, Employment and Health Benefits: A Connection at Risk
NIH, 2013, U.S. Health in International Perspective: Shorter Lives, Poorer Health
NIH, 2021, Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care
Unconventional Medicine, Chris Kresser, 2019
Michael A. Morrisey, PhD, 2013, Health Insurance, Second Edition